Chronic Pain and Inflammation
If you’ve ever dealt with chronic pain, you know it can feel like a relentless companion. Waking you up in the middle of the night. Keeping you from enjoying family time. Feeling short with your partner or kids. Missing out on your parenthood. Consuming your waking hours hunch over the laptop looking for answers. Gaslighting you into thinking “it’s all in your head”. And making you feel crazy when the doctors tell you “eat healthy and exercise” or “lose weight and you’ll feel better”.
But what if I told you that the root cause might not be something you’d expect?
Chronic inflammation—often the silent culprit behind chronic pain—can be heavily influenced by what you choose to consume. For those who have spent years on medication, the idea that food could be the answer might sound, well, too good to be true. Too simple. But with anti-inflammatory eating and personalized protocols like LEAP, relief is closer than you think. Let’s dive deep into chronic inflammation, its link to pain, and how the right food choices can make all the difference.
Understanding Chronic Inflammation and Its Link to Pain
Chronic inflammation isn’t your everyday redness and swelling. I mean, that IS also inflammation, but not what I’m talking about. The acute redness and swelling typically leads to healing. Think of chronic inflammation as a slow burning fire smoldering in your body, quietly wreaking havoc on your cells, tissues, and organs. When inflammation lingers, it can lead to a variety of issues—from digestive distress to chronic skin flares, and yes, pain.
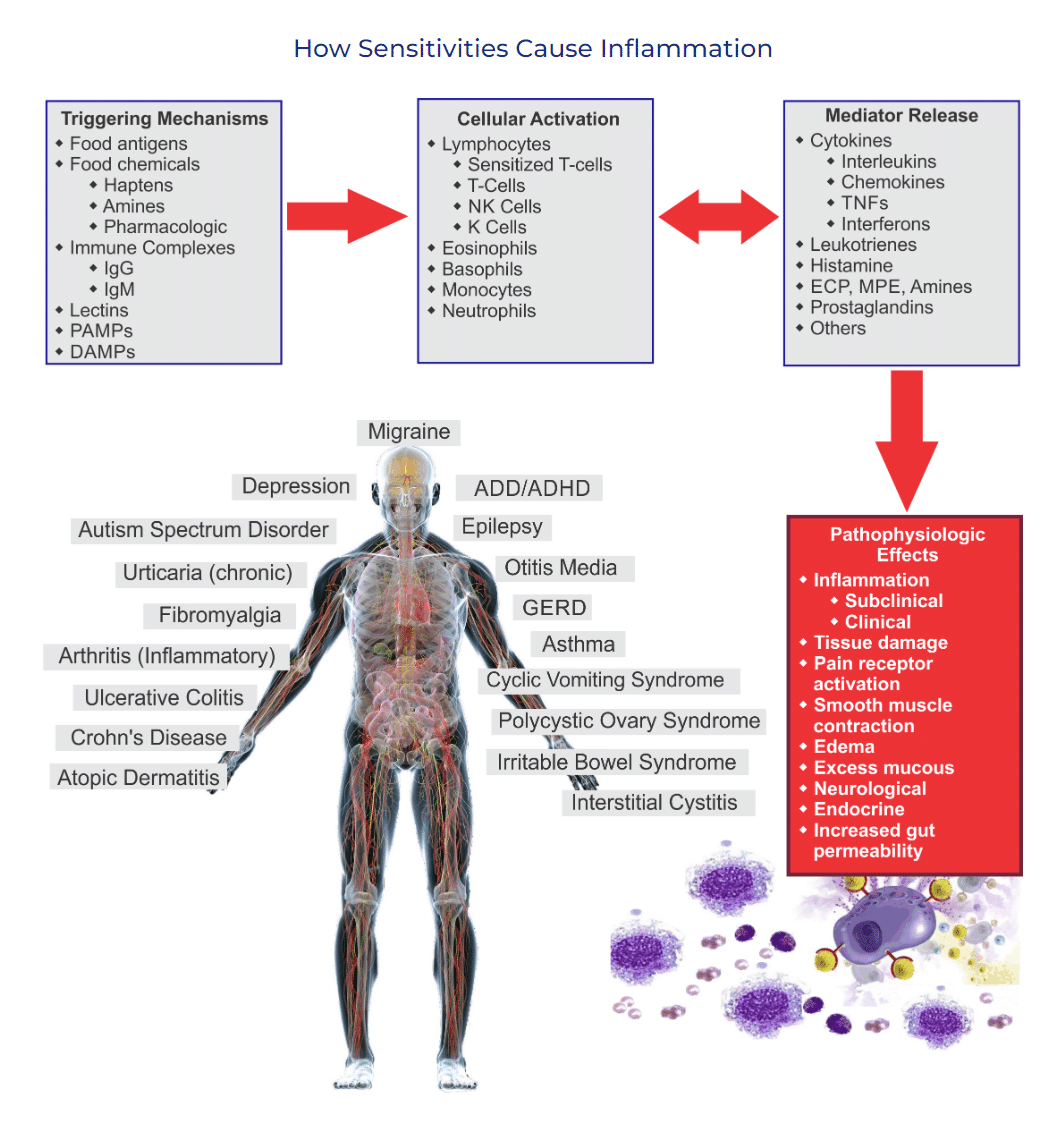
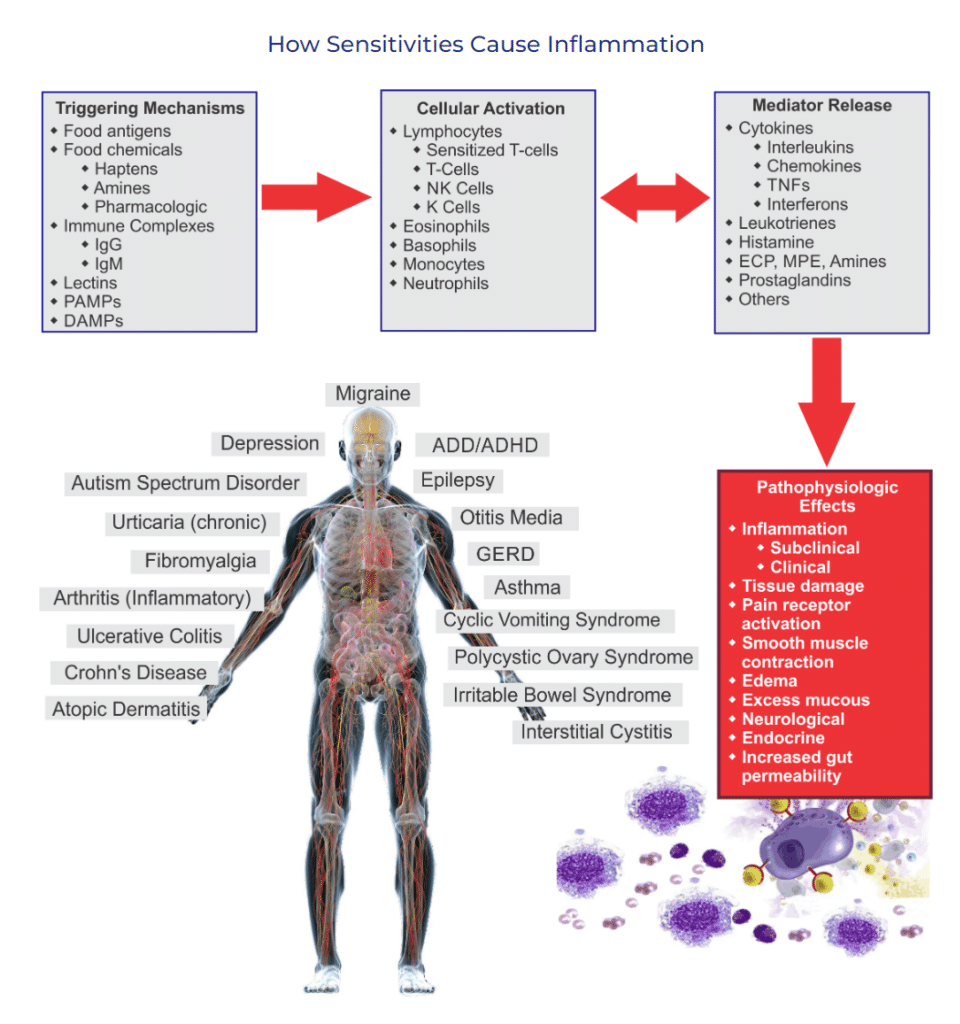
But why pain? Well, inflammation triggers the release of certain chemicals in the body that can irritate nerves and cause discomfort. Over time, the release of these inflammatory mediators (aka: toxins) cause constant irritation and can lead to conditions like arthritis, migraines, fibromyalgia, IBS, and even neuropathy (1). Actually way more symptoms too!
Chronic pain and inflammation can become part of a vicious cycle, with pain itself often leading to more inflammation. And the usual suspects like NSAIDs and other pain relievers? They’re like fire extinguishers—helpful for a moment but unable to keep the flames from reigniting. AND your body can become reactive to some of the ingredients in the very medicine that should be helping you.
The Role of Reactive Foods: Are They Fueling the Fire?
Here’s where food comes into play. Just as certain foods can help douse the flames, others can unintentionally throw fuel on the fire. Reactive foods are those that trigger your immune system, leading to the release of inflammatory mediators— like the wind…essentially fanning the flames within. And, surprise! These reactive foods can be highly personal. While your best friend or partner might thrive on tomatoes and almonds, you might feel worse after a meal featuring the same ingredients.
Unpopular opinion: Ginger, Salmon, and Olives are NOT anti-inflammatory for ALL bodies all the time.
Through MRT (Mediator Release Testing), I’m able to pinpoint which foods are problematic for each individual and which ones are leading to chronic pain and inflammation. The test measures your immune system’s response to 176 different foods and food chemicals, helping to identify specific triggers. Using these results, I curate a personalized LEAP (Lifestyle, Eating, and Performance) protocol, which weaves in foods that nourish rather than antagonize your body. I like to consider this approach more like an inclusion diet vs elimination diet. You can learn more about the MRT test and LEAP protocol HERE.
What Are the Toxins and Inflammatory Mediators
I am not a cellular biologist nor an immunologist. So this is just my understanding of these toxins and how they relate to chronic inflammation.
Chronic pain and inflammation can lead to the release of various harmful substances, often called “inflammatory mediators” or “toxins,” which can contribute to tissue damage and exacerbate pain and other symptoms. Here are some key toxins and inflammatory mediators commonly associated with chronic inflammation:
Cytokines
- Examples: Tumor Necrosis Factor-alpha (TNF-α), Interleukins (IL-1, IL-6, IL-17), and Interferon-gamma (IFN-γ)
- Function: Cytokines are signaling proteins that regulate inflammation. In chronic inflammation, they can promote prolonged inflammatory responses, contributing to pain and tissue damage.
Prostaglandins
- Function: These lipid compounds are involved in the inflammatory process and are often responsible for causing pain, fever, and swelling. Prostaglandins play a significant role in sensitizing nerve endings, which can increase the perception of pain.
Reactive Oxygen Species (ROS) and Free Radicals
- Examples: Superoxide, hydrogen peroxide, hydroxyl radicals
- Function: These are unstable molecules that can damage cells, proteins, and DNA. Chronic inflammation leads to an overproduction of ROS, which can cause oxidative stress and further contribute to cell and tissue damage.
Nitric Oxide (NO)
- Function: Although nitric oxide is essential for immune response and blood vessel regulation, excessive levels can lead to oxidative stress and inflammation, potentially resulting in damage to tissues and cells.
Histamines
- Function: Histamines are typically associated with allergic reactions, but they are also involved in inflammation. They increase blood flow to affected areas, which can cause swelling, itching, and discomfort. Chronic inflammation can lead to persistent release of histamines, which contributes to ongoing symptoms.
Matrix Metalloproteinases (MMPs)
- Function: MMPs are enzymes that break down proteins in the extracellular matrix. While they play a role in tissue repair, their excessive release during chronic inflammation can lead to tissue degradation, especially in conditions affecting joints and connective tissues.
Lipopolysaccharides (LPS)
- Function: LPS are toxins released by certain bacteria, particularly in cases of gut dysbiosis or leaky gut syndrome. They can trigger an immune response and inflammation, especially when they enter the bloodstream, leading to systemic inflammation and exacerbating chronic conditions.
C-Reactive Protein (CRP) and Other Acute Phase Proteins
- Function: CRP is produced by the liver in response to inflammation and can promote an inflammatory response. High levels of CRP in the bloodstream are markers of systemic inflammation and are linked to an increased risk of chronic diseases.
All of these mediators have a functional role in our bodies. But we need them to do a GOOD job when necessary. Not when we eat a carrot, piece of bread, or even drink ginger tea!
The MRT test doesn’t measure each specific mediator – but we can get a really good idea of how reactive your blood (and your cells) get with 176 foods and food chemicals.
Why Personalized Anti-Inflammatory Eating Works When Meds Fall Short
I’m not a doctor, nor should this be taken as medical advice, so take this for what it is – one dietitian’s professional opinion. Medication can be effective at dulling pain, but it rarely addresses the underlying cause. And SOMETIMES can even be counter-effective if the body has become reactive to certain ingredients (like Blue Lake 1, or Red 40). So while it might feel best to reach for an anti-inflammatory, food may be your best option to address chronic pain and inflammation.
Food has more power to influence chronic pain and inflammation at the cellular level. By removing reactive foods, you’re effectively cutting off the fuel supply to that slow burning fire (and the mediator release to cause chronic pain and inflammation). And without that steady supply, inflammation begins to die down. Over time, this reduction in inflammation translates into less pain, improved energy, and better overall health.
Imagine this: You’ve spent years chasing relief, and it turns out that what you needed all along was to let go of foods that don’t agree with your body. And while anti-inflammatory eating can take time and patience, the rewards are more than worth it. Not only are you likely to experience less pain, but you’ll also be supporting your body’s natural ability to heal. That’s what I call a win-win!
Getting Started with Anti-Inflammatory Eating
If you have been struggling with chronic pain and inflammation, here’s my loving reminder: anti-inflammatory eating isn’t about perfection. It’s about progress. Begin by noting how certain foods make you feel. Keep a food journal, jot down your symptoms, and pay attention to patterns.
And, of course, if you’re ready to take a deeper dive, the MRT test offers a scientific roadmap to guide you through the process.
At the end of the day, the journey toward relief from chronic pain and inflammation doesn’t have to be lonely or overwhelming. With compassionate guidance and a bit of patience, you can reclaim your health—and finally put out that persistent fire within.
I invite you to follow me on social media to learn more about me and how I can help you relieve your chronic pain and inflammation.
Case Studies/Testimonies for Chronic Pain and Inflammation
Finding Relief from Rheumatoid Arthritis Through Personalized Diet with Sara
Amy K. was diagnosed with Rheumatoid Arthritis (RA) in 2016 and struggled for years with diet, exercise, and mobility challenges. After disappointing results with a nutritionist, Amy’s rheumatologist recommended she work with a dietitian, leading her to Sara. Amy appreciated Sara’s engaging personality and commitment to addressing her health concerns, rather than just managing symptoms.
Amy enrolled in the LEAP program and diligently followed the protocol. Though initially skeptical, she began noticing significant improvements in her chronic pain and inflammation after two months. Eventually, Amy woke up one day feeling substantially better, with decreased pain and a newfound understanding of how specific foods affected her body. Her blood tests confirmed a remarkable drop in inflammation—23 points lower—demonstrating the positive impact of her dietary changes.
Amy highlights the value of working with a knowledgeable, science-based professional like Sara over self-guided methods. Despite the time and financial commitment, she found the experience transformative, learning how to prioritize her health and navigate food choices that support her long-term well-being.
Transforming Health and Wellness with Sara’s Guidance
Sarah B. came to Sara seeking relief from chronic pain and inflammation, fatigue, brain fog, digestive issues, and skin concerns. Within weeks of starting her personalized plan, Sarah noticed significant improvements across the board—her pain diminished, energy returned, and her skin, hair, and nails began to heal.
Sarah was particularly impressed by Sara’s holistic and pressure-free approach. Despite having celiac disease and previously avoiding gluten, Sarah discovered with Sara’s guidance that certain “healthy” foods she consumed regularly were actually triggering her symptoms. Through careful evaluation, Sara helped Sarah identify and eliminate these reactive foods, leading to noticeable relief and a feeling of transformation.
Unlike previous experiences, Sarah appreciated that weight loss was not the primary focus; instead, Sara prioritized how Sarah felt over any numbers on the scale. This approach provided a refreshing sense of freedom and a renewed confidence in making nourishing choices.
Sarah found Sara to be understanding, nonjudgmental, and supportive throughout the process. Reflecting on her journey, Sarah recommends Sara wholeheartedly, emphasizing the long-lasting impact of investing in one’s health with a knowledgeable guide.
Are you ready to feel well?
If you’re next stop is to look for relief for your chronic pain and inflammation, I invite you to book in a free call with me HERE.
Or check out The Collective – my private guidance and group support program. Where you’re longer alone with your symptoms and where we heal together.
Most of all…. be well.
Love, Sara.